Abstract
Introduction
Platelets are small anucleated granular cytoplasmic fragments of megakaryocytes. While thrombocytosis begets thrombotic events, thrombocytopenia leads to bleeding disorders. Hence, an accurate platelet count is necessary for planning transfusions in cases of thrombocytopenia. The immunological-based gold standard platelet estimation is not routinely feasible, and automation remains a faster alternative. We audited the platelet count and platelet indices generated by our five-part analyzer and compared the correlation with the manual count done on Leishman stained slides.
Materials and Methods
This prospective cross-sectional study was done in the Central Laboratory of Sir Sunderlal Hospital, BHU. All the samples sent for Complete Blood Count (CBC) which fitted the criteria of slide review because of platelet count or indices flagging were included. The exclusion criteria being the same as sample rejection criteria of the lab wherein the samples are either clotted, hemolyzed or improperly labelled. All samples analyzed were in 2ml K2 EDTA vacutainers.
We collected data from 1795 samples, in whom slides were reviewed, from a total of 19028 samples processed for CBC. The platelet count on the machine and manual counts were recorded. The automated 5-part analyzer works on the principle of impedance for platelet count. It also provides platelet indices like mean platelet volume (MPV), plateletcrit (PCT), and platelet distribution width (PDW). The manual count was done on thin Leishman-stained smears. The formula used for manual platelet count was [20,000 x average platelet count in 10 oil immersion fields] lacs/ cumm.
All the data collected were coded and entered in Microsoft Excel sheet which was re-checked and analysed using SPSS v 22. Normality of distribution was checked using Kolmogorov-Smirnov test. Pearson Chi-square test was used for comparing categorical variables between groups. Spearman correlation was done to find out correlation between two quantitative variables. A p value of <0.05 was considered statistically significant.
Results
The most prevalent age group encountered was that of the young adults (15-47 years); 927 (51.6%) patients. This was followed by older adults (48-63years) and geriatric patients (>64years), 21.1% and 13.7%, respectively. 9.2% patients were of pediatric age group (1-14 years), neonates (<28days) were 3.5% and infants (<1years) being 1.1%. 60.1% were males, and the rest were female patients.
The median Total Leukocyte count (TLC) was 7.16(4.22-12.91) x 109/l, median Red Blood Cell count was 3.65(2.88-4.45) x 1012/l and median Hemoglobin was 100(79-120) gm/l.
The median machine platelet count was 53(30-75) x 109/l, while median manual platelet count was 70(40-110) x 109/l. Thrombocytopenia was the commonest cause of slide review accounting up to 82.2% (1476) cases, followed by 15.2% (273) with average platelet count, and 2.6% (46) with thrombocytosis.
The median MPV was 9.80(8.30-11.20) fl, median PDW was 17.50(16.80-18.20) and median Plateletcrit was 0.05(0.02-0.08) %. 12.7% of patients had MPV >12fl, rest were within normal range.
The overall correlation of manual and machine platelet count was 0.861 with p<0.01. Discrepancies were only seen in those flagged as thrombocytopenia on the machine. 91.4% of those had thrombocytopenia on both methods, while 8.6% (138) patients had a normal count on the manual assay.
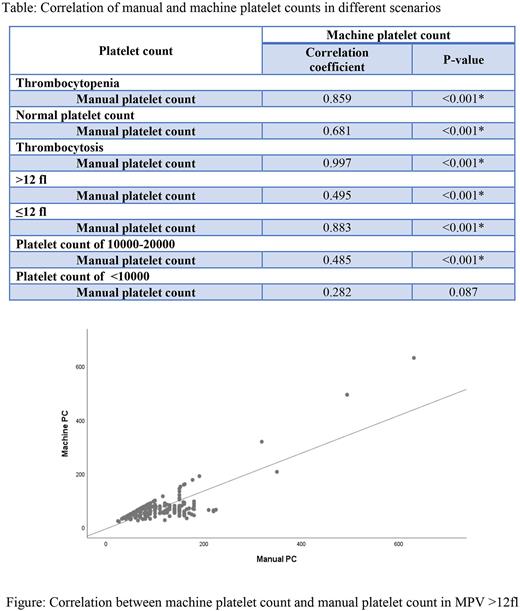
There was correlation coefficient between the manual and machine counts was 0.859, 0.681 and 0.997 (p value <0.001), in patients with thrombocytopenia, those within normal range and those with thrombocytosis, respectively.
MPV >12fl was detected more commonly in patients with thrombocytopenia 173 (75.9%), followed by those with normal counts 53 (23.2%) and only 2 (0.9%) patients with thrombocytosis.
As expected, the correlation [0.495; p value <0.001] was poor in those with MPV >12fl, while it was 0.883 (p value <0.001) in the rest with normal MPV.
The correlation was poorer in patients with marked thrombocytopenia, i.e., count ≤ 20 x 109 /l. The correlation was 0.485 (p value <0.001) in those with counts between 10 - 20 x 109 /, and 0.282 (p value 0.087) in those with counts <10 x 109 /l.
Conclusion
Patients with marked thrombocytopenia and high MPV (>12fl) on machine should be undergo slide review. Transfusion-related decisions can then be made based on the manual count, thus avoiding unnecessary transfusions and exposure.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal